
CareTeam is a research project and partnership between Southampton City Council, the University of Southampton and Nquiringminds. It is partly funded by Innovate UK, the UK’s innovation agency.
CareTeam has developed an adult support digital platform that comprises a mobile app and household and personal sensing technologies. This platform wants to support independent living and help carers support their loved ones more efficiently and effectively. CareTeam aims to help adults who currently receive home care to remain independent, comfortable and active, living in their own homes without feeling isolated and unmotivated.
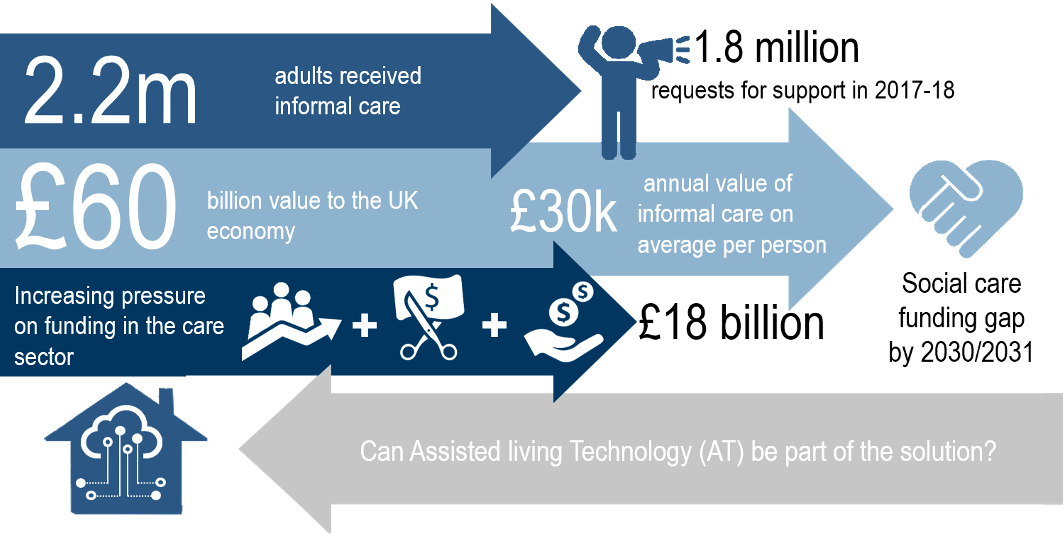
Over the period 2016-2017, local councils in the UK have received around 1.8 million of new requests for support (1). The Gross Current Expenditure of Local Authorities on Adult Social Care in the UK for the same period, reached £17.5 billion with the majority of funds spent in long term care (77.6% or £13.6 billion) (1). The cost of care for people aged 65 and over is around £7 billion with 25.5% (~£4.5 billion) spent on physical support (1). At the same time the unpaid carers were supported with £166 million and an additional £196 million was spent for assistive equipment and technology (1).
The 2011 UK Census data indicated that the number of unpaid carers in the UK is around 6.5 million of whom 2.5 million provided more than 19 hours of unpaid care per week (2). More importantly, there is a link between the deterioration of the self-health of the unpaid carers and the total hours of care they provided (3). The Gross Value Added from unpaid “informal” carers has been estimated to be around £56.9 billion in 2014 (4). This is three times more than the current UK Local Authorities’ social care budget. Furthermore, as the currently active informal carers grow older, it is expected that part of the unpaid care they provide will eventually shift to formal care. Carers’ stress and fatigue is likely to lead to an increasing number of informal carers requiring health support from the NHS before the age of 65 compounding the pressure of health services. Such demographic changes and the austerity affecting Local Authority budgets will have a big impact on the quality of life of adults in receipt of care, their families, social care and public health.
*This introduction was originally presented in the conference paper “Person-centric activity profiles for homecare support” at the CIBSE Technical Symposium, London, UK, 12-13 April 2018.
CareTeam Digital platform and sensors
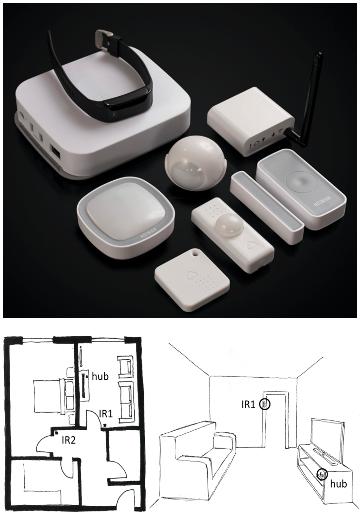
CareTeam is an app that can be used on a smart phone or tablet. It comes with different sensors that can be installed in the home. Carers can then use the platform to check remotely and identify potential issues.
- App includes functions such as: Secure group messaging, Calendar, Updates and to do lists and Contacts.
- Sensors can measure:
Temperature and relative humidity, movement of people, specific activities, such as whether a hot drink has been made, or a door opened
The monitoring kit at this stage comprises a communication hub, 2 passive infrared movement sensors (IR) and an accelerometer tag (left). The movement sensors (IR) are installed at places with high expectations of movement such as the living room and the hallway that leads to the bedrooms and bathroom (right).
Household Trial
The ASDP approach links the activity schedule of the adult in receipt of care (e.g. carer visits) with in-situ monitoring in homes. As part of the CareTeam IoT approach to care, two passive infrared (PIR) motion sensors were installed at the lounge and the hallway of the houses in the trial. The selection of these rooms was the result of a combination of privacy issues, high likelihood of movement and activity expectations. The activity in these rooms was expected to be representative of the daytime occupancy (i.e. lounge) and the night-time activity (i.e. hallway that connects bedrooms with toilet and kitchen).
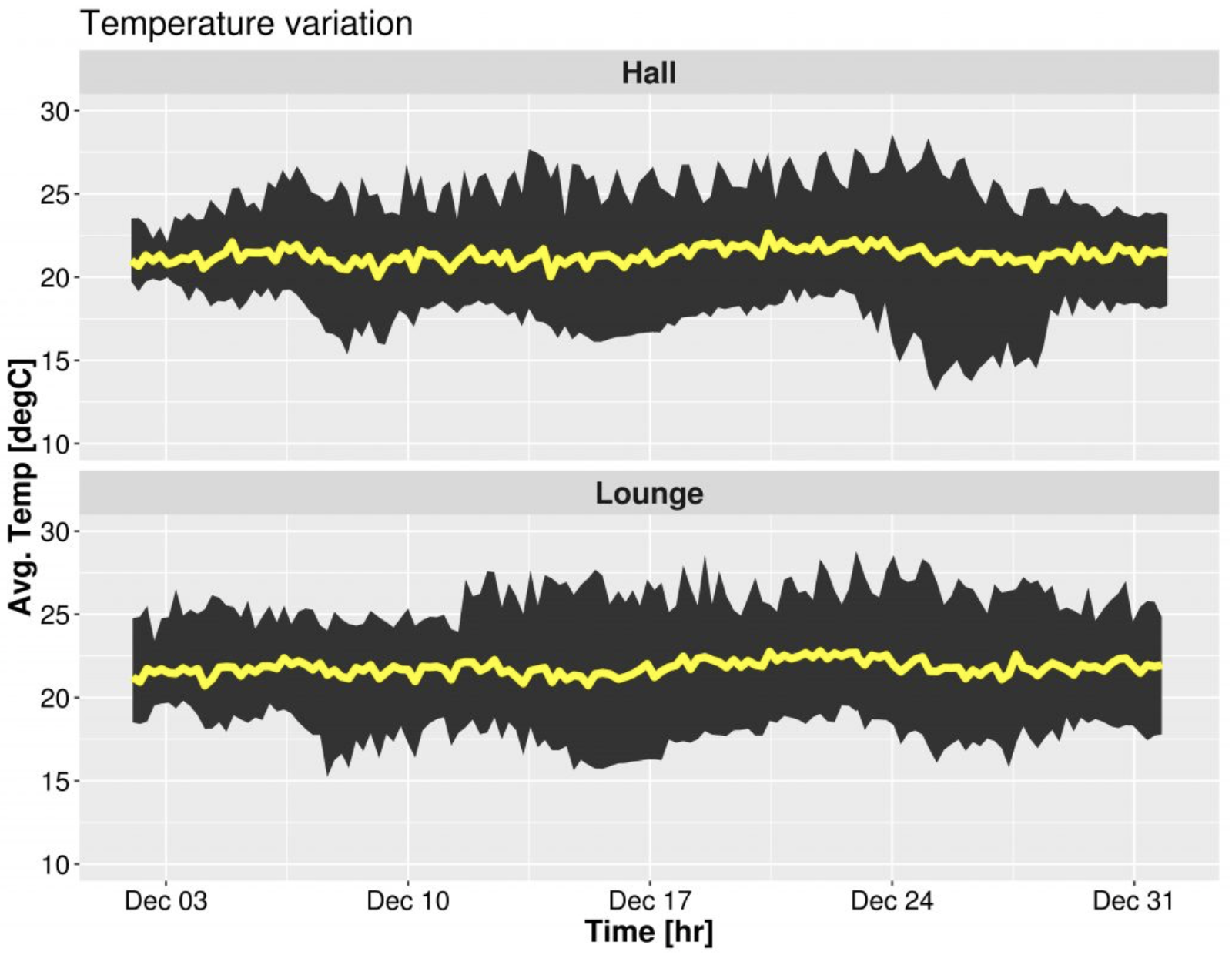
Hourly average air temperature range in the hall (top) and the lounge (bottom) during December 2018. The yellow line shows the average temperature from all houses in the trial. The above figure shows the hourly average temperature from the homes in the trial during December 2018.
The app displays the latest sensors’ readings and the users can configure custom alerts on movements’ frequency and temperature thresholds.
Three data processing steps were undertaken:
- Raw data from the sensors were evaluated against the user settings for movement and temperature set points (human in-loop approach).
- Investigation of similar patterns between groups with common characteristics, i.e. “Typical” occupancy behaviour profiles for groups of people with similar care requirements.
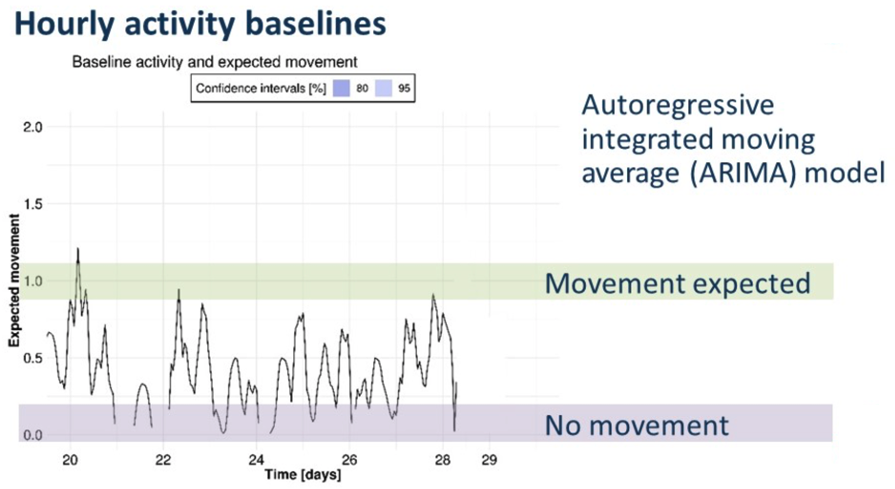
- Trend analysis and forecasts to develop an adaptive activity baseline and track changes to the expected patterns (human out of loop).
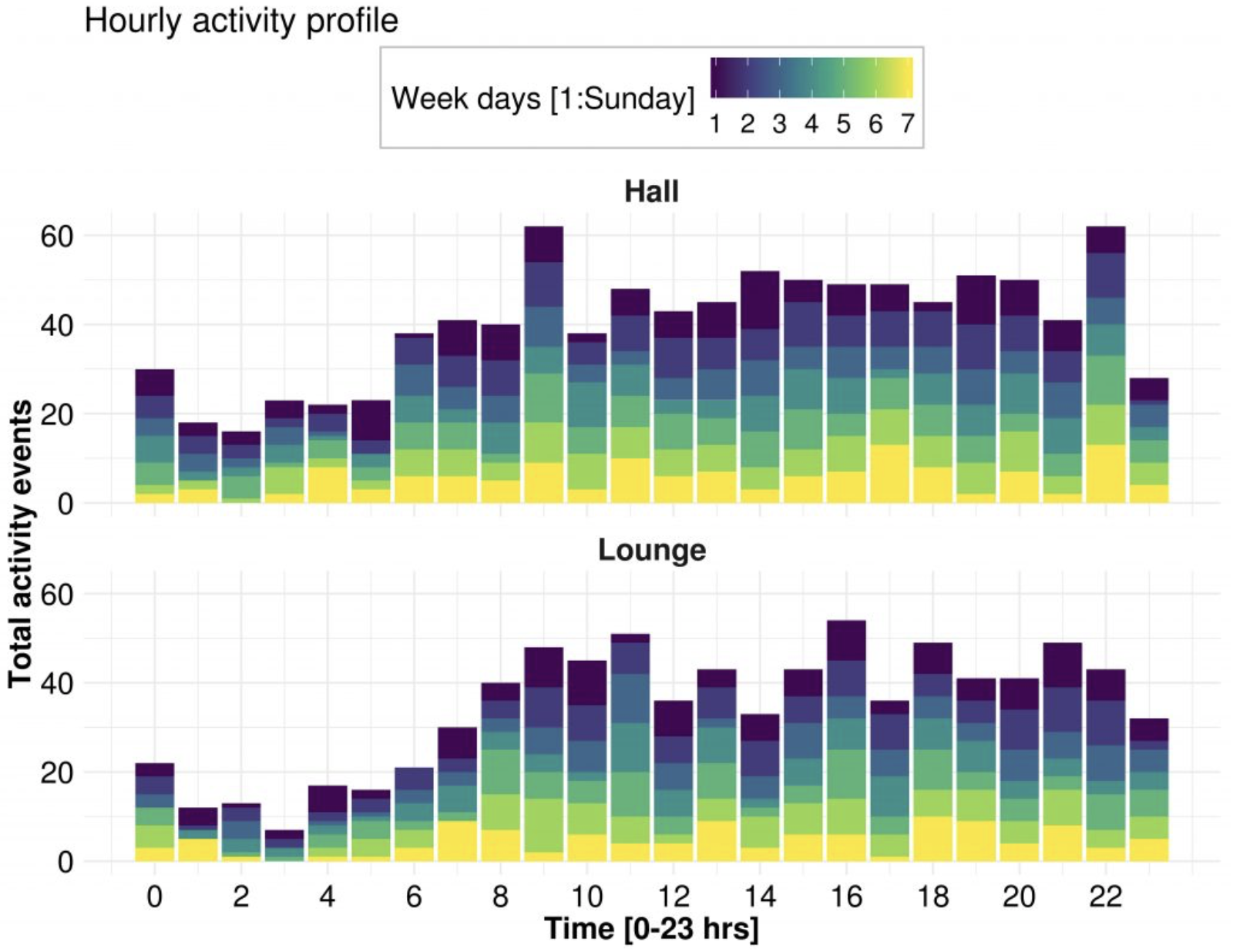
The combination of these three processes or steps are aimed at enabling the generation of proactive warnings and help the carers assess changes in short and long term monitored behaviours. Total hourly activity detected in hall (top) and lounge (bottom) for each day during December 2018. The black box marks the night-time activity cluster.
The feedback during the ongoing CareTeam trial highlighted the lack of coordination of care. This has a large impact on a person’s care and their families’ views and expectations for formal support. In the near future, IoT will have prominent role to play in the coordination of care to achieve increasing care efficiency and communication between formal and unpaid care providers.
- This first trial although small in sample size, concludes that the IoT design concepts may fail to take into account the needs and skills of the users. In particular, care professionals and those who receive care, all seem to prefer very simple app features and targeted functions that can help them accomplish predefined tasks with less effort. This aspect may be critical to IoT implementation in care provision as the users of the technology are not aspired by the modernity, and technical specifications but they are mostly attracted by the trustworthiness and inclusivity features.
- Several informal carers and care organisations were interested in the CareTeam background sensing capabilities and the proactive warnings based on household specific occupancy profiles.
- The initial findings from this study suggest that in the context of adult care, the care needs of the person who receive care and their independence from carers can be important determinants of the movement trends in the house. Interestingly, during night-time, the activity levels indicated that the movement pattern is related to the care needs of the participants in the trial with those having higher care needs showing less activity than those with low care requirements.
Baseline activity (black line) and 24hr forecasts of expected movement. Dates shown are in December 2018.
This study evaluated the use of household specific ARIMA models for the development of baseline occupancy profiles from PIR motion observations. Short-term projections were successfully created to establish an “expectation” of activity at specific times. Future work will cover larger sample size and will aim to integrate a probabilistic approach to the occupancy profiles and evaluate the merits of different machine learning approaches in their use with occupancy related time series in the context of care at home.
CareTeam aspires to introduce a new paradigm for care coordination and the use of IoT for the development of person specific, adaptive and evolving background data interpretation and proactive care-awareness to support independent living.
For more information on the app, the sensors and ways to participate visit the CareTeam trials website.
References
1. Adult Social Care Statistics, NHS Digital. Adult Social Care Activity and Finance Report: Detailed Analysis. England 2016-17. UK: NHS Digital, part of the Government Statistical Service, 2017.
2. Office for National Statistics, National Records of Scotland, Northern Ireland Statistics and Research Agency. Provision of unpaid care. 2011 Census aggregate data. UK Data Service (Edition: June 2016). 2016.
3. Stokes P. The gender gap in unpaid care provision: is there an impact on health and economic position?2013 28 November 2017. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandwellbeing.
4. Webber D, Payne CS. Compendium, Household satellite accounts 2005 to 2014. Chapter 3: Home produced ‘adultcare’ services.: UK Data Service; 2016.

